Bony outgrowths, called bone spurs or osteophytes, which form when the joints of the spine calcify, may also cause these symptoms.
Anterior cervical discectomy with fusion is an operation that involves relieving the pressure placed on nerve roots and/or the spinal cord by a herniated disc or bone spurs – a condition referred to as nerve root compression.
Through a small incision made near the front of the neck (i.e., the anterior cervical spine), the surgeon:
- Removes the intervertebral disc to access the compressed neural structures
- Relieves the pressure by removing the source of the compression
- Places a bone graft between the adjacent vertebrae, and
- In some cases, implants a small metal plate to stabilize the spine while it heals.
Discectomy involves removing all or part of an intervertebral disc. The term discectomy is derived from the Latin words discus (flat, circular object or plate) and -ectomy (removal). Spinal fusion involves placing a bone graft between two or more opposing vertebrae to promote bone growth between the vertebral bodies.
Why is it done?

Pressure placed on neural structures, such as nerve roots or the spinal cord, by a herniated disc or bone spur may irritate these neural structures and cause: pain in the neck and/or arms; and lack of coordination, numbness or weakness in the arms, forearms or fingers. Pressure placed on the spinal cord as it passes through the neck (cervical spine) can be serious since most of the nerves for rest of the body (e.g., arms, chest, abdomen, legs) have to pass through the neck from the brain.
Patients who suffer from these symptoms are potential candidates for this surgery.
Surgery

An understanding of what an anterior cervical discectomy with fusion involves will help you to approach your surgery and recovery with confidence.
Incision
You will lie on your back on the operating table and be given anesthesia. Once asleep, your neck area is cleansed and prepped. If a fusion is planned and your own bone will be used, the hip area is also prepped to obtain a bone graft. If a donor bone will be used, the hip incision is unnecessary.
Exposure
A 2-inch skin incision is made on the right or left side of your neck. The surgeon makes a tunnel to the spine by moving aside muscles in your neck and retracting the trachea, esophagus, and arteries. Finally, the muscles that support the front of the spine are lifted and held aside so the surgeon can clearly see the bony vertebrae and discs.
Removal
With the aid of a fluoroscope (a special X-ray), the surgeon passes a thin needle into the disc to locate the affected vertebra and disc. In order to remove the damaged disc, the vertebrae above and below the disc must be held apart. Your surgeon first inserts a spreader into the body of each vertebra above and below the disc to be removed. Gentle tension is placed on the spreader to separate the two vertebrae.
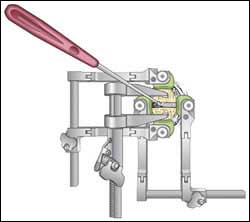
The outer wall of the disc (annulus) is cut (Fig. 3). The surgeon removes about 2/3 of your disc using small grasping tools, and then looks through a surgical microscope to remove the rest of the disc. The posterior longitudinal ligament, which runs behind the vertebrae, is removed to reach the spinal canal. Any disc material pressing on the spinal nerves is removed.
Material Placement
Bone grafts come from many sources. Each type has its advantages and disadvantages.
- Autograft bone comes from you. The surgeon takes your own bone cells from the hip (iliac crest). This graft has a higher rate of fusion because it has bone-growing cells and proteins. The disadvantage is the pain in your hipbone after surgery. Harvesting a bone graft from your hip is done at the same time as the spine surgery. The harvested bone is about a half-inch thick – the entire thickness of the bone is not removed, just the top half layer.
- Allograft bone comes from a donor (cadaver). Bone-bank bone is collected from people who have agreed to donate their organs after they die. This graft does not have bone-growing cells or proteins, yet it is readily available and eliminates the need to harvest bone from your hip. Allograft is shaped like a doughnut and the center is packed with shavings of living bone tissue taken from your spine during surgery.
- Bone graft substitute comes from human-made plastic, ceramic, or bioresorbable compounds. Often called cages, this graft material is packed with shavings of living bone tissue taken from your spine during surgery.
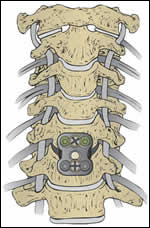
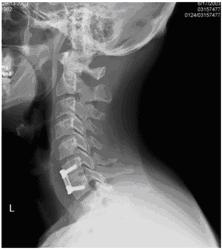
Stabilization
A metal plate may be implanted on the front of the cervical spine to increase the stability of the spine immediately after surgery. Surgeons use these implants to decrease the amount of time that you have to wear a cervical collar after surgery and to increase your chances of developing a solid fusion. An X-ray is taken to verify the position of the bone graft and the metal plate and screws.
Closure
The spreader and retractors are removed. The muscle and skin incisions are sewn together with sutures. Steri-Strips or biologic glue is placed across the incision. The operation is completed when your surgeon closes and dresses the incision.
Recovery
Your surgeon will have a specific post-operative recovery/exercise plan to help you return to normal life as soon as possible. The amount of time that you have to stay in the hospital will depend on this treatment plan. You will normally be up and walking in the hospital by the end of the first day after the surgery.
It is important that you discuss the potential risks, complications, and benefits of spinal surgery with your doctor prior to receiving treatment, and that you rely on your physician’s judgment. Only your doctor can determine whether you are a suitable candidate for this treatment.
What are the results?
Anterior cervical discectomy is successful in relieving arm pain in 92 to 100% of patients [3]. However, arm weakness and numbness may persist for weeks to months. Neck pain is relieved in 73 to 83% of patients [3]. In general, people with arm pain benefit more from ACDF than those with neck pain. Aim to keep a positive attitude and diligently perform your physical therapy exercises.
Achieving spinal fusion varies depending on the technique used and your general health (smoker). In a study that compared three techniques: ACD, ACDF, and ACDF with plates and screws, the outcomes were [3]:
- 67% of people who underwent ACD (no bone graft) achieved fusion naturally. However, ACD alone results in an abnormal forward curving of the spine (kyphosis) compared with the other techniques.
- 93% of people who underwent ACDF with bone graft placement achieved fusion.
- 100% of people who underwent ACDF with bone graft placement and plates and screws achieved fusion.
Recurrent neck pain is common. The key to avoiding recurrence is prevention:
- Proper lifting techniques
- Good posture when sitting, standing, moving, and sleeping
- Appropriate exercise program
- An ergonomic work area
- Healthy weight and lean body mass
- Positive attitude and relaxation techniques (e.g. stress management)
- No smoking.