Cervical disc replacement has made great strides since the first cervical disc was approved by the United States Food and Drug Administration (FDA) in 2007.
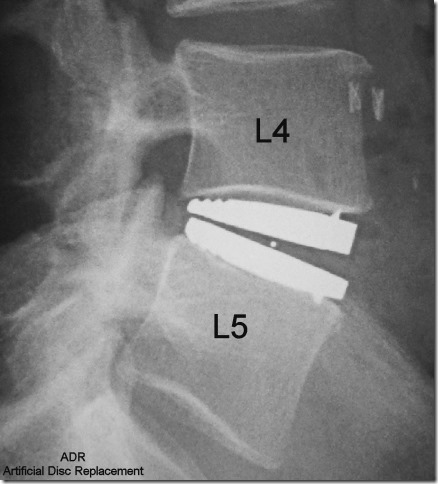
Artificial Disc Replacement: Treatment for Degenerative Disc Disease
Artificial disc replacement surgery is indicated for patients with severe degenerative disc disease (DDD).
Degenerative disc disease is a condition that can occur in the neck or low back and cause significant pain. As we age, the discs typically dehydrate and become more brittle. As the discs degenerate, they flatten out and can develop cracks in the outer layer, known as the annulus fibrosus.
Degenerative discs can cause pain in patients for several reasons:
- The annulus can come in contact with nerve fibers or pain receptors, called nociceptors.
- The nerve fibers can grow into the cracks of these discs and cause pain.
- Portions of the nucleus, or core of the disc, can bulge out and push on these fibers.
- There are proteins in the nucleus that are chemically irritating to the nerves and can cause pain.
For some patients, removal of the offending disc alone is not enough. Spinal fusion, which immobilizes the painful disc, has long been the standard of care in patients who don’t respond to non-surgical treatments. The theoretical benefits of disc replacement are to preserve motion and reduce abnormal stresses at the disc above and below the surgery.
Lumbar Artificial Disc Replacement

What makes artificial disc surgery so challenging is that unlike a ball and socket joint, such as the hip, the disc is a complex joint with motion in several planes. It is difficult to emulate the natural motion of the disc while maintaining stability.
In 2004, the FDA approved the first lumbar disc replacement. Use of the device skyrocketed as the implant gained popularity, fed by surgeon interest, patient demand, and optimism over this new treatment modality.
Unfortunately, much of the research showed few benefits over spinal fusion. Disc replacement leaves you with a mobile device that may wear out during your lifespan. In many patients, the indications were over-extended (that is, this treatment was given to patients who may not have been ideal candidates), and the device had to be removed or fused from behind.
Several patients didn’t experience as good outcomes as expected. This led to insurance companies in the US declining coverage and the reduced use of lumbar disc replacement.
Cervical Artificial Disc Replacement
Cervical disc replacement, however, has become much more popular. This is in part to better patient selection, lower forces in the neck, and safer revision strategies.
The January 2009 issue of Spine contained a report from researchers at Washington University in St. Louis. A group of spine surgeons conducted a study to determine how artificial disc replacement compares to spinal fusion in patients with cervical degenerative disc disease. The spine surgeons reported that most patients who received an artificial disc had a speedier recovery than those who underwent a spinal fusion. The surgeons concluded that the patients who had artificial disc replacement surgery recovered just as well—or better—than those who had spinal fusion.
The first artificial cervical disc was approved in 2007. While cervical disc replacement still suffers from some of the stigma of lumbar disc replacement, it has been better received in the spine community as a whole.
To view images of cervical and lumbar artificial discs, visit our other article about artificial disc replacement surgery.
If you suffer from severe disc problems, talk to your doctor about whether you are a candidate for surgery. If you are, spinal fusion might not be your only option—artificial disc replacement may also successfully treat your back or neck pain.
(Source: SpineUniverse)