Osteoporosis, a disease that gradually weakens bones and causes them to become brittle, affects an estimated 10 million Americans, according to the National Osteoporosis Foundation. Left untreated, osteoporosis can progress painlessly until a bone breaks. Along with hip and wrist fractures, severe osteoporosis can cause compression fractures in the spine. This occurs when the bony block, or vertebral body, in the spine collapses – causing severe pain, deformity, and loss of height. It can also lead to nerve compression. Compression fractures occur in more than 700,000 patients per year in the United States, are more frequent than hip fractures, and often result in prolonged disability. Pain medication, bed rest, bracing or invasive spinal surgery used to be the only treatment options. But now we have vertebroplasty and kyphoplasty.
Vertebroplasty
Vertebroplasty was originally developed in France in 1986 and has been further refined and available in the US since 1991. Vertebroplasty is a minimally invasive, non-surgical procedure that is designed to relieve the pain of compression fractures. Vertebroplasty literally means fixing the vertebral body. In addition to relieving pain, those vertebral bodies that are weakened but not yet fractured can be strengthened, thus preventing future problems.
How is vertebroplasty performed?
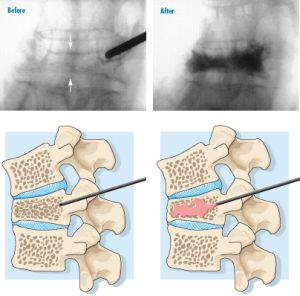
Under general anesthesia, or sometimes under sedation, a special bone needle is passed slowly through the soft tissues of the back. Image guided X-ray, along with a small amount of x-ray dye, allows the position of the needle to be seen at all times. A small amount of orthopaedic cement, called polymethylmethacrylate (PMMA), is pushed through the needle into the vertebral body. PMMA is a medical grade bone cement that has been used for many years in a variety of orthopaedic procedures.
The cement is sometimes mixed with an antibiotic to reduce the risk of infection, and a powder containing barium or tantalum, which allows it to be seen on the X-ray. When the cement is injected, it is like a thick paste, but it hardens rapidly. Usually each vertebral body is injected on both the right and left sides, just off the midline of the back. Within a few hours, patients are up and moving around. Most go home the same day.
Kyphoplasty
Kyphoplasty is a newer treatment for patients immobilized by the painful vertebral body compression fractures associated with osteoporosis. Like vertebroplasty, kyphoplasty is a minimally invasive procedure that can alleviate up to 90% of the pain caused by compression fractures. In addition to relieving pain, kyphoplasty can also stabilize the fracture, restore height, and reduce deformity.
How is kyphoplasty performed?
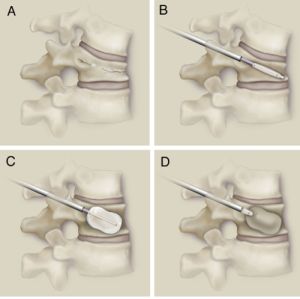
Kyphoplasty is performed under local or general anesthesia. Using image guidance X-rays, two small incisions are made, and a probe is placed into the vertebral space where the fracture is located. The bone is drilled and a balloon, called a bone tamp, is inserted on each side. These balloons are then inflated with contrast medium (to be seen using image guidance X-rays) until they expand to the desired height and are removed. The balloon does not remain in the patient. It simply creates a cavity for the cement and also helps expand the compressed bone. The spaces created by the balloons are then filled with PMMA, the same orthopedic cement used in vertebroplasty, binding the fracture. The cement hardens quickly, providing strength and stability to the vertebra, restoring height, and relieving pain.
Benefits
Limitations in the traditional treatments of vertebral compression fractures have led to the refinement of such procedures as vertebroplasty and kyphoplasty. These procedures provide new options for compression fractures and are designed to relieve pain, reduce and stabilize fractures, reduce spinal deformity, and stop the “downward spiral” of untreated osteoporosis.
Additional benefits of these procedures include:
- short surgical time
- only general or local anesthesia required
- average hospital stay is one day (or less)
- patients can quickly return to the normal activities of daily life.
Both vertebroplasty and kyphoplasty utilize a cement-like material that is injected directly into the fractured bone. This stabilizes the fracture and provides immediate pain relief, in many cases. Kyphoplasty has the additional advantage of being able to restore height to the spine, thus reducing deformity. After either procedure, most patients quickly return to their normal daily activities. While vertebroplasty and kyphoplasty are encouraging developments, it remains essential that osteoporosis sufferers seek medical help and learn about ways to treat their condition, as well as ways to prevent future problems.