SED is a method of spinal surgery that announced the beginning of the period of minimally invasive spinal neurosurgery in the 1990s. Since then, with the advance of technology and acquiring new knowledge about disc ailments, endoscopic spinal neurosurgery has been rapidly evolving worldwide. The concept of this type of surgical procedure has derived from relatively unfavorable results of present conventional spinal surgery and the fact that patients who have undergone traditional surgeries have difficulty with a prolonged return to work and their normal activities. The main principle of this method is a minimally invasive approach that enables painless surgeries performed under local anesthesia, surgeries performed on all types of disc hernia, outpatient surgery, rapid recovery and timely start of physical therapy, and prompt return to normal activities.
Benefits of SED compared to standard open spine surgery
- Local anesthesia is much safer than general anesthesia
- No bleeding or need for transfusion
- Only the abnormal disk material is removed so there’s less chance of disc space collapse
- Your recovery should be much quicker since nothing other than your skin is cut
- The endoscope provides more light and better magnification than open surgery
- We are able to see the traversing and exiting nerve roots better

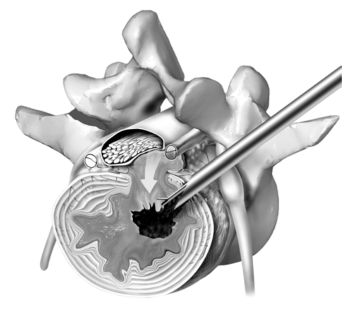
Selective Endoscopic Discectomy™ (SED™) is a minimally invasive spine surgery technique that utilizes an endoscope to treat herniated, protruded, extruded or degenerative discs that are a contributing factor to leg and back pain. The endoscope allows the surgeon to use a “keyhole” incision to access the herniated disc. Muscle and tissue are dilated rather than being cut when accessing the disc. This leads to less tissue destruction, less postoperative pain, quicker recovery times, earlier rehabilitation, and avoidance of general anesthesia. The excellent visualization via the endoscope allows the surgeon to selectively remove a portion of the herniated nucleus pulposus contributing to the patient’s leg and back pain.
Thermal annuloplasty is an adjunctive procedure that uses bipolar electro-thermal energy (radiofrequency and/or laser) to ablate or depopulate the sensitized pain nociceptors in the annulus, ablate any inflammatory/granulation tissue that has grown into the annulus, and to shrink and tighten the stretched or torn collagen fibers of the annulus. The annulus is the outer portion of the disc and is composed of many concentric layers that are arranged similarly to the plies of a radial tire. Thus, the weakened annulus or defect left by the disc herniation is contracted and possibly sealed from within the disc.
This combination procedure and the endoscopic system used to perform the unique procedure is pioneered and developed by Dr Anthony Yeung, with instruments developed with the Richard Wolf Instrument Company (YESS – Yeung Endoscopic Spine Surgery system). This state-of-the-art technique is an evolution from the technique originally described by Parviz Kambin called Arthroscopic Microdiscectomy (AMD).
At Aksis Special Hospital, we follow the philosophy of the world’s leading minimally invasive spinal surgeons, and combine their methods, knowledge and experience. Some of them have already been mentioned: Dr. Anthony Yeung, Dr. Martin Knight, late Dr. Thomas Hoogland, Dr. Sang-Ho Lee, Dr. Hansjorg Leu, etc.
There are other electro-thermal techniques utilized for painful, bulging degenerative discs and annular tears called IDET and Nucleoplasty/Coblation. SED™ and thermal annuloplasty, however, is NOT the same. SED™ is different because it is a visualized endoscopic surgical method (like knee arthroscopy) that is designed to visualize the pathoanatomy of the disc, spinal canal, and adjacent nerves. These other percutaneous procedures are only fluoroscopically guided and are termed “blind” procedures. Consequently, SED™ can be used for pain caused by contained or non-contained (extruded) disc herniations, and sometimes works as well for discogenic back pain that is not responsive to non-surgical treatment. Patients who are otherwise destined for fusion may have a minimally invasive alternative for pain relief without fusion in selected patients.
Description and procedure
The endoscope enables the neurosurgeon a so-called “keyhole” approach to disc herniation. Muscles and tissue are stretched and expanded instead of being cut. This surgical method leads to less tissue destruction, less postoperative pain, shortens recovery time, faster rehabilitation, and the danger of general anesthesia is nonexistent. The excellent visualization provided by the modern endoscope enables the neurosurgeon to selectively remove the disc herniation causing the patient’s back and leg pain.
During this operation, the neurosurgeon can also perform thermal radiofrequency annuloplasty and minimize the chances of recurrent disc herniation at the operated level. Inflammatory altered pain sensors as well as inflammatory granulation tissue located in the disc sheath are neuromodulated, leading to a reduction in postoperative pain. This innovative approach to performing surgery at our Special Hospital is performed by top Croatian spinal neurosurgeons, who have received the necessary training for such procedures in the world’s most famous centers where endoscopic spine neurosurgery was developed.
Endoscopic discectomy is an operation performed under so-called local potentiated anesthesia, without sedation, which allows for constant interaction and communication between the neurosurgeon and the patient with the aim of making the operation as successful as possible. After the patient is prepared, the place of entry of the endoscope is determined diascopically, local anesthesia is administered to the patient, and the endoscope is inserted through a half-centimeter incision. The surgery itself, depending on the specifics of each individual patient, lasts between 30 minutes and an hour and a half.
After surgery, the patient rests under the constant supervision of the medical staff and is ready to leave the hospital in two to three hours. It’s important to emphasize that the endoscopic approach to the treatment of spinal diseases removes the cause of pain, i.e. the pressure on the neural structures, while preserving the remaining healthy part of the disc. This approach to spinal treatment minimizes all the negative aspects of classical treatment, such as permanent painful sensations, neurological deficits, and scar changes.